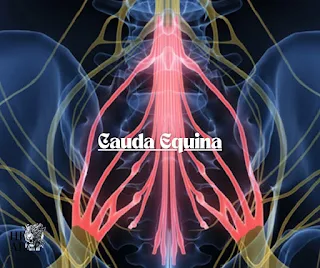
Cauda Equina Syndrome
Understanding Cauda Equina Syndrome
Cauda equina syndrome refers to the compression of a cluster of nerve roots known as the cauda equina. These nerves serve as pathways for electrical signals in your body and are located at the base of your spinal cord, resembling a horse’s tail. The cauda equina nerves play a crucial role in facilitating leg movement and sensations, as well as controlling the urinary bladder.
When these nerves are compressed, it can lead to various distressing symptoms, including pain, weakness, and incontinence. If left untreated, this syndrome has the potential to cause permanent damage, including paralysis. Timely intervention can help prevent irreversible harm.
Is Cauda Equina Syndrome Life-Threatening?
While cauda equina syndrome is not considered life-threatening, it can significantly impact your overall health and quality of life. Symptoms may involve difficulties related to urination, defecation, and sexual function. Immediate surgery may address some of these symptoms.
Exploring the Types of Cauda Equina Syndrome
Types of Cauda Equina Syndrome
- Acute Cauda Equina Syndrome: This form of the syndrome is characterized by the sudden onset of severe symptoms. In such cases, surgical intervention is typically required within 24 to 48 hours.
- Chronic Cauda Equina Syndrome: The term “chronic” is used to describe long-lasting cauda equina syndrome, which can manifest in two scenarios: a. If you’ve experienced symptoms of cauda equina syndrome for an extended period before seeking medical attention, it is classified as chronic. b. In cases where surgery fails to restore nerve function, and permanent damage persists, the condition is labeled as chronic. Individuals with chronic symptoms typically experience them for the remainder of their lives.
Timely emergency surgery may help prevent permanent damage. If you exhibit symptoms, it’s crucial to consult with a healthcare provider.
Classifications of Cauda Equina Syndrome
- Complete Cauda Equina Syndrome: This category of cauda equina syndrome results in urinary and/or bowel retention or incontinence. Retention implies an inability to urinate or defecate, while incontinence means an inability to control urination or defecation. Approximately 60% of individuals with cauda equina syndrome experience complete symptoms.
- Incomplete Cauda Equina Syndrome: Affecting the remaining 40% of individuals with the syndrome, incomplete cauda equina syndrome presents with symptoms like altered bladder and bowel sensation without retention or incontinence. This means you may have difficulty sensing the need to urinate or defecate, or the sensation may be stronger than usual.
The Rarity of Cauda Equina Syndrome
Experts estimate that cauda equina syndrome affects roughly 1 in 65,000 people, affecting both males and females.
Symptoms and Causes
How Does Cauda Equina Syndrome Develop?
Several factors can lead to the compression of the nerve roots within the cauda equina, including:
- Congenital anomalies during birth.
- Lumbar spinal stenosis.
- Lower back injuries resulting from accidents or trauma, such as car accidents or gunshot wounds.
- Herniated disks in the lumbar region, which is the most common cause.
- Complications arising from postoperative lumbar spine surgery.
- Spinal arteriovenous malformations (AVMs).
- Spinal hemorrhages.
- Spinal infections like meningitis or inflammation.
- Spinal lesions or tumors.
Recognizing the Symptoms
Key indicators that you might be experiencing cauda equina syndrome include:
- Altered sensations in the buttocks, inner thighs, legs, and hips, often referred to as the “saddle area.”
- Back and leg pain, often presenting as sciatica.
- Sexual dysfunction.
- Urinary and/or fecal incontinence.
- Urinary retention.
- Weakness or paralysis in the lower extremities.
Additional symptoms may accompany these warning signs, such as lower back pain, tingling, numbness, or pain in the lower limbs (paresthesia), and reflex abnormalities. If you experience these symptoms, it’s essential to consult a healthcare provider promptly. You may undergo tests to assess the presence of cauda equina syndrome and may be referred to a neurosurgeon or orthopedic spine surgeon for potential surgical intervention.
Diagnosis and Tests
How Is Cauda Equina Syndrome Diagnosed?
The diagnosis of cauda equina syndrome involves a comprehensive assessment by your healthcare provider. This evaluation encompasses a discussion of your symptoms, a physical examination, various tests, and imaging studies. During the physical examination, you may be asked to perform tasks such as standing, sitting, walking on your heels and toes, bending in different directions, and lifting your legs while lying down. This helps your healthcare provider assess your stability, sensation, strength, reflexes, alignment, and motion. In some cases, a rectal examination may also be conducted to evaluate anal muscle function.
Furthermore, your healthcare provider may order specific imaging tests, including computed tomography (CT) scans, magnetic resonance imaging (MRI), and myelograms. These tests allow for the visualization of bones, nerve roots, the spinal cord, and any displacement of spinal structures due to herniated disks, bone spurs, or tumors.
A definitive diagnosis of cauda equina syndrome is typically made when two sets of symptoms are present:
- Bowel, bladder, and/or sexual dysfunction.
- Paresthesia in the “saddle area.”
Questions for Diagnosis
Your healthcare provider may ask you various questions to facilitate an accurate diagnosis, including:
- Details about your symptoms.
- Duration of symptom onset.
- Information about your current medications.
- History of spine-related injuries.
- Clarification of the most distressing symptom.
- Previous experience with herniated disks.
Management and Treatment
Addressing Cauda Equina Syndrome
In cases of acute cauda equina syndrome, immediate surgical intervention is imperative. Timely surgery is usually performed within 24 hours to relieve the compression on nerve roots and facilitate their healing. This surgical procedure is known as a lumbar laminectomy.
To improve bowel and bladder control, certain medications like hyoscyamine (Levsin®), oxybutynin (Ditropan®), and tolterodine (Detrol®) may be prescribed. Physical therapy and occupational therapy may also be recommended to aid in regaining strength and managing everyday activities post-surgery.
Prevention
Reducing the Risk
While it may not be possible to prevent all the causes of cauda equina syndrome, you can take steps to reduce the risk of a herniated disk, a common underlying cause of this condition. Consider the following preventative measures:
- Avoid wearing high-heeled shoes, as they can lead to spinal misalignment.
- Quit smoking and refrain from using tobacco products, as they can weaken spinal disks.
- Engage in regular exercise, particularly activities that strengthen the back and abdominal muscles.
- Lift objects correctly by bending your knees and maintaining proper back alignment, instead of bending at the waist.
- Maintain a healthy body weight to reduce extra pressure on the lower back.
- Practice good posture to minimize strain on the spine.
- Incorporate regular stretching into your routine, especially after prolonged periods of sitting.
Outlook and Prognosis
Long-Term Effects
If you experience symptoms of cauda
equina syndrome, it is crucial to seek immediate medical attention. Early surgery is often necessary, as it offers the best chance of preventing long-term complications. Swift surgical intervention reduces the duration required for nerve healing. While surgery may aid in nerve recovery, it may take some time to fully regain control over bowel and bladder functions, alleviate pain, and address weakness. These improvements occur gradually over months or even years.
Living with Cauda Equina Syndrome
Self-Care and Support
If you are experiencing cauda equina syndrome symptoms, the most important step you can take is to consult with a healthcare provider. Additionally, ongoing support from healthcare professionals, including physical therapists, occupational therapists, and mental health experts, is valuable. Consider seeking assistance from family and friends as you navigate the challenges posed by the syndrome. Support is essential as you may require ongoing care and rehabilitation.
Questions for Your Healthcare Provider
When discussing cauda equina syndrome with your healthcare provider, consider asking the following questions to ensure you receive comprehensive information:
- What specific type of cauda equina syndrome do I have?
- Can you clarify the classification of my cauda equina syndrome?
- How urgently do I require surgery?
- What is the expected duration of the surgical procedure?
- How long will I need to stay in the hospital following surgery?
- Is a herniated disk contributing to my condition?